Intubation: What You Need To Know To Be Good At It
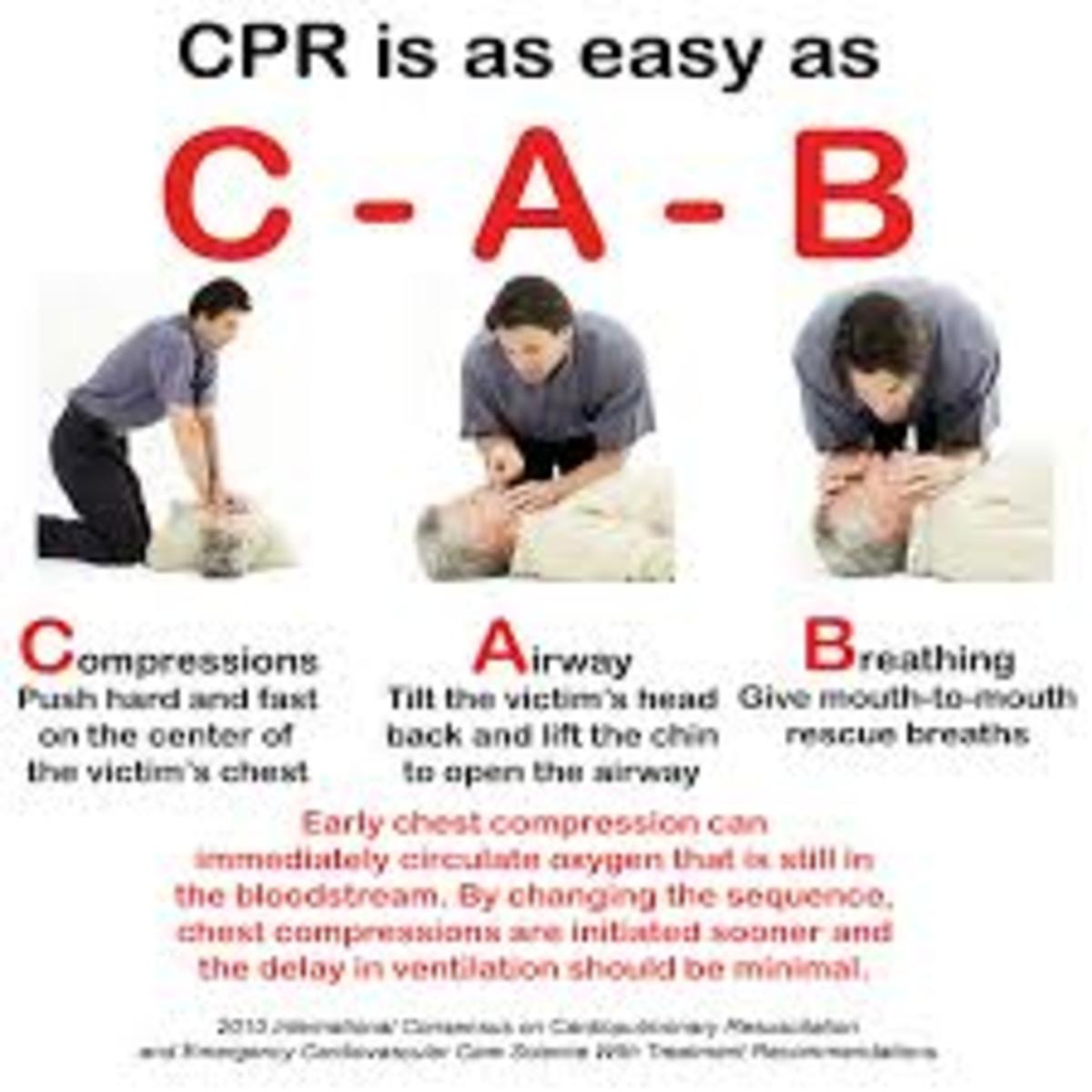
One of the most important duties of a respiratory therapist during a “code blue” resuscitation attempt (Code) is intubation. Intubation is the act of placing an endotracheal tube (E.T. tube) into the patient’s trachea, establishing a patent airway through which the patient can be connected to a life support ventilator. If this procedure is not performed quickly and correctly, it is much more likely that the resuscitation attempt will be unsuccessful, regardless of other life saving measures performed. For most therapists, especially new graduates, the pressure to master this procedure is enormous due to the fact that it is truly of life and death importance.
This article, written by a registered respiratory therapist with roughly twenty years of experience, provides suggestions that will make you much more effective and confident to perform this procedure when the need arises. It is assumed the reader will be well-versed with and trained in the various technicalities associated with this procedure, therefore, this article is written in the less “academic” tone of an older, experienced respiratory therapist giving advice to a new practitioner.
The Reality of the Situation
As a new therapist, you have worked hard to prepare. You have studied and re-studied your craft, working your way through the formidable process of passing the National Board of Respiratory Care’s credentialing examinations, and now find yourself on your first job. With a mix of excitement and trepidation, you are ready to take on all of the responsibilities you have trained for. You know that, at any moment, the calmness of the day can be interrupted with the sudden, overhead page, “CODE BLUE IN THE E.R”! This is the moment when every member of the resuscitation team immediately drops whatever they are doing and rushes to the announced location to, literally, fight for the life of a dying human being. It could be a new-born baby who suddenly stops breathing, a little girl who stepped out in front of a car, a teen-ager who suffered a gunshot wound, or an elderly man suffering a heart attack. You never know what kind of medical emergency may present itself from one moment to the next. In a heartbeat, you find yourself in a whirlwind of activity in which each member of the team is expected to perform their particular duties with life saving precision. No pressure, right?
Below, I am going to explain exactly how to be prepared and equipped to confidently perform an intubation. I will cover all of the mental “bullet points” you’ll need to remember every time, and I will offer you important thoughts to consider about the actual, “nitty-gritty” technique of intubating a human, as opposed to a training dummy. I will, also, give you important information you need to be aware of as a member of the resuscitation team.
First Things First
Before anything else, preparation is absolutely necessary in order to perform an effective intubation. This means that every single member of your department or resuscitation team (most importantly, YOU) must take fundamental, unfailing responsibility for two things. First, that every disposable supply and permanent piece of equipment needed to perform this procedure is present and in good working order before the need for them arises. And second, that each and every time this cache of equipment or supplies is used, care is taken to replace supplies to par level and insure the equipment is cleaned, sterilized, and ready to go for the next emergency. This is of utmost importance! When you are suddenly called to a Code, it is not the time to discover that a vital piece of equipment is missing, or that someone forgot to replace a particular size E.T. tube that you desperately need for this particular patient. Remember, someone’s life is in your hands. Being part of the resuscitation team, even something as seemingly mundane as restocking supplies after a Code can become a matter of life and death urgency for the next person who has to use that equipment, and you never know, that person might be you. Trust me, when you need something in a Code, you need it right now! Resolve yourself right now to never allow your own carelessness to be the reason a resuscitation attempt is unsuccessful. Restock supplies and verify the presence of clean, working equipment after every single Code, no exceptions!
“Code Blue!”
When a “Code Blue” is called, you drop whatever you are doing and quickly move to the designated location. A somewhat stunning sense of surprise and urgency arises within you as you make your way to the scene, inevitably encountering other team members rushing to perform their individual tasks. It quickly becomes a very exciting and energetic atmosphere, and it is not uncommon for other stressors to present themselves as you are sucked into this whirlwind of activity. It may be a screaming family member distraught from the sight of their loved one having fallen, ashen-faced, into cardio-pulmonary arrest. It may be the presence of staff members quickly hurrying family and visitors from the immediate area as they search your face with helpless urgency, knowing you are here to save the life of their loved one. Maybe your patient was the victim of a horrendous accident and, as you enter the room, you are momentarily stunned by the amount of blood or physical carnage you are encountering. The point is, whatever the particular circumstances, you will very suddenly be dealing with a great deal of stress, emotion, and energy, within moments of having been calmly going about your day. We all have our own ways of dealing with high stress situations, some better than others, but my best advice is to avoid getting caught up in the emotional excitement of it all and focus on your task at hand. You are the team member that is here to establish and maintain a patent airway, after which you will provide the ventilatory support essential for this person’s survival. Focus on the simple fact that you are here to work on “an airway”, mentally taking the stance that you are here as a trained healthcare professional performing a medical procedure. From this mental standpoint, it is much easier to maintain the focus necessary to perform effectively in such a high-stress environment. Treat the Code more like a science project and don’t get caught up in the emotionality of the fact that a human being is dying. You will have all the time in the world, after the Code, to mentally and emotionally process what you have just taken part in. During the Code, a calm, focused, professional demeanor will serve you and the patient best.
What to Focus On
Now that we have addressed the necessity of remaining calmly focused in the high-stress environment of a Code, let’s get down to the “nitty-gritty” of exactly what you should focus on. In my decades of experience, a mental checklist has evolved which, I find, will have me ready to handle any situation. I would like to share with you the mental process I go through each and every time I know an intubation is about to be performed. Wherever the Code is to be performed, my first thoughts are to insure the presence of the necessary supplies and equipment which I, then, quickly prepare for the procedure. Below, I will explain in order the process you will need to go through.
First and foremost, (avoiding all of the surrounding drama and excitement) I immediately verify that a suction machine is present, whether it is a plug-in-the-wall type apparatus or a freestanding suction machine. I make sure it is plugged in if necessary, and I turn it on, being sure to verify the presence of working suction. I quickly make sure it is properly set up with a disposable reservoir along with all of the necessary tubing, including both a Yankeur style handle and an appropriately sized, flexible, deep suction catheter. It is a very common occurrence during a Code to find that the patient’s mouth, oropharyngeal space, and airway are filled with vomit, organic debris, or blood. All of this must be removed in order to see the necessary anatomical landmarks you will need to perform the intubation, as well as to clear the airway for adequate oxygenation and ventilation. Even if suction is not required initially, it is very common for a patient to vomit during the procedure. Having the suction on and running with the Yankeur style handle attached and in reach is of utmost importance in order to clear the mouth and minimize aspiration. Once the E.T. tube is placed, you will likely need to deep suction the airway through the E.T. tube with a flexible suction catheter that should be readily available nearby.
After verifying the presence of properly working and fully equipped suction, my next thought on the mental checklist is to verify the presence of a bag-valve device, or “ambu-bag” (as well as an appropriately sized face mask) with which to “bag” the patient, or provide life saving breaths, both before and after the intubation. It is important to take the “ambu-bag” out of its packaging, open it up, hook it up to a running oxygen flow meter, and verify that it is working properly and that the face mask is present. Never assume that the face mask is included as some manufacturers differ in what is included in the packaging. Remember, it is your task to verify the presence and proper working order of all equipment pertaining to the airway!
Once the presence of properly working suction and ambu-bag (with mask) is verified, you will need to quickly prepare your laryngoscope with properly sized blades, and obtain properly sized E.T. tubes, stylettes, and E.T. tube holders. Due to the fact that the intubation tools and supplies required for each, particular patient are necessarily determined by the size of the patient, you will need to quickly find out, either by direct observation or, possibly, by report from incoming ambulance personnel, all of the pertinent patient size information in order to determine appropriate equipment and supply sizes to prepare. If the patient is not already present for direct observation, you will most likely have some general details provided by incoming emergency medical personnel or, perhaps, police.
At this stage it is important to be methodical. First, obtain the laryngoscope handle. Next, obtain a properly sized laryngoscope blade (based on the information you have already obtained regarding the size of your patient) and attach the blade to the handle, locking it into place. At this point, make sure to verify that the blade “fits” the handle. It is not uncommon that a hospital will have purchased several different brands of laryngoscope equipment that are not necessarily compatible with one another. During cleaning and sterilization processes the wrong blade may have been erroneously returned to the wrong crash cart or intubation box, resulting in the incompatible laryngoscope blade not fitting onto the handle properly. Believe me, this type of thing happens, and your methodical attention to detail can discover this error and correct it before the critical moment of the actual intubation. So, be sure to verify the blade fits the handle properly. Once the blade is locked onto the handle, verify that the light on the end of the blade comes on very strongly and brightly. It is absolutely vital that this light is working properly in order to see once the device is placed into the patient’s dark, wet, fleshy mouth and throat. If the light emitted is dull, flickering, or of low intensity, consider replacing the batteries in the handle or replacing the light bulb. Also, make sure the tiny, removable light bulb is screwed in tightly to the end of the blade. A loose bulb falling off in the middle of the intubation not only eliminates the vitally necessary light, but it also introduces a foreign body that can easily obstruct or damage the airway. Some of the newer laryngoscope blades are designed with the lights permanently integrated into them in order to avoid these types of hazards. It is a good idea but, when the light fails in these types of blades you will have to throw away the entire blade, which can be less than cost effective.
Once you have your laryngoscope and properly sized blades prepared, select your E.T. tubes. Speaking informally here, I would like to offer you some rough guidelines for choosing the right sizes. Again, this is a rough guideline, meant to offer you some general information that I think you will find helpful. I have found that, for an average-sized adult (male or female), a 7.5 E.T. tube is a good starting point. That being said, airway sizes are, often, anatomically dissimilar so, it is best to gather a range of about three sizes for a single patient. For example, if my patient is an average-sized adult, I will prepare three E.T. tubes, sizes 7.0., 7.5, and 8.0. The purpose here is to have the size you think is going to be right, plus one larger and one smaller. It is not uncommon to estimate needing a certain size and, once you actually visualize the trachea, find that you need a slightly different sized tube, whether larger or smaller. The goal is to try to get the largest size E.T. tube fitted into the airway in order to have the least amount of airway resistance once the patient is on the ventilator. Imagine breathing through a straw. The smaller the straw, the harder and more uncomfortable it will be to breathe through. I have stated above that an average-sized person will usually be good with a 7.5. E.T. tube. This is a good guideline to help you, but it needs to be applied with a healthy dose of your own observation skills. If the patient is an average sized adult but has a particularly small frame, you may want to consider starting with a 6.5 or a 7.0 and, if average-sized but with a wide-shouldered, stocky build, be prepared to go with a size 8.0 E.T. tube. I will tell you that, with enough experience, you will eventually be able to correctly judge the correct adult E.T. tube size about 95% of the time just by performing a quick visual examination of the patient. The 7.5 starting point is a good general reference for adults. All of this being said, however, it is important to have a large variety of E.T. tube sizes close by in order to be prepared for any odd situation that comes along. For instance, victims of smoke inhalation or, perhaps, an insect sting may present with significant swelling in their airway requiring you to use a much smaller E.T. tube than they would normally require. It is very important to stay sharply focused on each, particular patient and remain flexible in your approach to establishing an airway despite whatever clinical challenges they present.
Children and infants obviously present a different size range than adult patients, so the above general guidelines for adults will be ineffective. Fortunately, most hospitals are now equipped with pediatric crash carts that have highly developed systems for quickly determining correct E.T. tube sizes for pediatric and neonatal patients. One such system I have found to be very easy to use is the measurement method. The child or baby is laid flat on a stretcher and measured from head to toe with a color-coded tape measure. After having found the correct, color-coded measurement, simply open the corresponding color-coded drawer on the crash cart and all of the properly sized equipment appropriate for that patient will be pre-packaged inside, including the E.T. tube. If you find yourself working in an environment where a system like this is unavailable, I will offer you another rough guideline that will assist you in selecting a properly-sized E.T. tube. Look at the child’s “little” finger and choose a tube that is close to that size in diameter. This will get you pretty close to the right size. Again, this is only a general guideline offered as an acceptable starting point for those unfortunate enough to not have one of the commercially available pre-sized systems. You should always be prepared to operate in the most meager of circumstances and, having this guideline has helped me on numerous occasions, therefore I offer it to you. Remember, with pediatrics and neonatal patients (just like adults), it is necessary to prepare a range of E.T. tube sizes in order to quickly change sizes, if needed, after directly visualizing the airway.
Once you have selected the properly-sized range of E.T. tubes appropriate for your patient you will need a few extra supplies from the crash cart in order to test the E.T. tube before use and, also, for the actual intubation. It’s a good idea to have a small, portable table onto which you can lay out all of these items for easy access. At this point, you will need to grab a 10cc syringe, several packs of K-Y Jelly, an appropriately-sized stylette, a roll of tape and, if available, a commercially manufactured E.T. tube holder. First, open the E.T. tube package on the proximal end (opposite the endotracheal cuff) maintaining, as much as possible, the sterility of the tube. Attach the 10cc syringe to the small cuff-inflator connection and inflate the cuff. Remove the syringe and verify that the cuff remains inflated with no leaks. Once proper cuff inflation is verified, deflate the cuff so it will be ready prior to the intubation attempt. Do this every time! The last thing you want is to intubate someone with a faulty E.T. tube causing you and the entire team to have to re-intubate the patient a second time. Not only is this entirely preventable occasion an unnecessary drain on everybody’s time and resources but, due to physiological things such as swelling and edema, there are no guarantees that you will be able to intubate the patient a second time. Make sure you test the cuff before every single intubation. Your patient’s life may depend on it.
Once you have verified the E.T. tube cuff is working properly, insert the stylette into the tube. In order to prevent damage to the airway, you never want the stylette to reach beyond the end of the E.T. tube. Position the distal end of the stylette to about one quarter inch less than the length of the E.T. tube and bend the stylette at the tube opening on the proximal end so it cannot pass any deeper than that. Some practitioners say they don’t prefer using a stylette. I respectfully disagree with them. The purpose of the stylette is to provide enough rigidity to the E.T. tube to effectively bend it into a shape conducive to placement into the trachea, and overcome any physical resistance against the tube from things like swelling or anatomical anomalies within the entrance to the airway. It is one of those things that you may not need but, if you do need it and don’t have it in place, you could fail to achieve the intubation. I use the stylette to bend the last two inches of the E.T. tube into a curve that makes it much easier to get into a deviated trachea, which you will find in about 30% of your patients (I will discuss this in more detail below). It’s a good habit to use the stylette every single time and I highly recommend that you do. There is nothing more frustrating than finding your E.T. tube is too pliable to enter a difficult airway, and then having to waste critical time applying a stylette that could have been there from the beginning. As stated above, preparation is key, and this is one of those areas where problems can be easily avoided by simply adopting the habit of placing the stylette into the E.T. tube beforehand, every single time.
Speaking of “entering the airway”, once your stylette is in place, coat the cuffed end of the E.T. tube with a generous layer of K-Y Jelly, maintaining sterility as much as possible. This lubrication is another very important factor in getting the E.T. tube to successfully enter the trachea. A non-lubricated cuff can be impossible to pass into the trachea and, if forced, can damage or tear the thin material of the cuff during intubation, which will cause you a great deal of trouble during your later attempt to ventilate the patient, necessitating re-intubation. I like to prepare and lubricate the E.T. tube as mentioned above and, then, carefully place the tube back into the sterile packaging just prior to the intubation attempt. I place the repackaged, lubricated, successfully-tested E.T. tube, with the stylette inserted and syringe attached, onto the table with the extra tubes, laryngoscope, blades, E.T. tube holder, ETC02 detector, and tape. I, also, recommend you have a pair of McGill Forceps available to help guide the tube, if necessary, especially in the event you determine naso-pharyngeal intubation will be required.
Please, note that all of the above mentioned preparations should be performed each and every time. Also, be aware that many pediatric and neonatal E.T. tubes are designed without a cuff in order to reduce the possibility of barotrauma (damage to fragile lung tissue due to the introduction of too much positive pressure into tiny airways). If you are using a cuffless E.T. tube for a small child, do everything mentioned above except, of course, verifying the cuff inflation.
Here is a brief summary of the above-mentioned things to focus on and prepare for each time intubation is to be performed:
1. Suction: plugged in, turned on, disposable reservoir and all necessary tubing properly assembled, both Yankeur-style handle (attached) and flexible suction catheters present, properly working suction verified.
2. Bag-Valve Device or “Ambu-Bag”: remove device from packaging, verify presence of a properly-sized face mask, expand bags that have been “folded down” for packaging, attach tubing to a running oxygen flow meter and verify the bag is in proper working order.
3. Laryngoscope and Laryngoscope Blades: in order to select proper sized blades, first ascertain the size of your patient, once selected- attach blade to laryngoscope handle, verify proper connectivity of blade and handle, observe the light bulb- if dim or flickering consider replacing batteries in the handle, ensure the bulb is screwed in tightly to end of blade (if applicable), ensure strong beam of light present, have both straight and curved blades of proper size present.
4. Supplies: properly sized range of E.T. tubes, 10cc Syringe, properly sized Stylette, K-Y Jelly, E.T. Tube Holder, Tape, McGill Forceps, ETC02 Detector, Stethoscope, ABG Kits, Universal Precaution Safety Equipment- gloves, goggles, disposable blood spatter gown, etc..
5. E.T. Tubes: select range of probable sizes rather than just one, maintaining sterility as much as possible test cuff inflation and viability, insert styllette into E.T. tube ensuring that it does not extend from tip of tube, lubricate cuff-end of tube with K-Y Jelly, using stylette bend tube into desired shape for easy insertion into trachea.
Memorize the above list, and I mean truly and thoroughly take it to heart, and you will have established a firm foundation with which to be able to set up for an effective, efficient intubation every single time the need arises. You will be able to approach your task with much more confidence knowing you are prepared for this procedure, and whatever special circumstance which may arise. Turn this attention to detail into your habitual thought process each and every time you prepare for an intubation. When it has become ingrained into your consciousness to the point that all of the above details can be accomplished in 30-45 seconds, you will find yourself much more able to focus on the actual technique of intubation itself, even in the most stressful of environments.
Man vs. Dummy
It takes most people a considerable amount of time to get enough real-life experience to have developed any real sense of technique when it comes to intubation. New practitioners will have read plenty about it and, therefore, will have a fairly well-developed cognitive understanding of what this procedure entails. They will have been afforded the opportunity to practice the technique on plastic intubation dummies and will have, also, been given time to thoroughly look over the tools of the trade (syringes, E.T. tubes, laryngoscopes, etc.). All this is a wonderful way to gain familiarity with the procedure but, I am sorry to say, intubating a practice dummy is nothing like intubating an actual human being. The practice dummy is dry, rigid, and non-pliable, which makes it difficult to access it’s airway with the laryngoscope. Often, a real human airway can seem fairly dissimilar due to its elasticity, and will look quite different from the rigid, plastic, perfectly placed anatomical landmarks of the dummy. Real human airways are, often, overly pliable and filled with wet, slime-filled, fleshy mouths, throats, and tongues that, when first viewed, rarely look or feel anything like the anatomical diagrams, pictures, and dummies you have been presented with during your training. In fact, about thirty percent of the people you are attempting to intubate will not have perfect oropharyngeal anatomical landmarks. The airway is often deviated to one side or the other or strangely positioned within the pharynx so that it doesn’t look at all like what you have been trained to look for. This can be a source of significant frustration for someone who has been training on the dummy and, when first attempting a real intubation, finds it to seem so different. I am not saying all of this to imply I am “anti-training-dummy”. They can, and do, serve a valuable purpose. I just want new practitioners to be prepared for the shock they may experience when they graduate from the training dummy to actual intubation.
Below, I will go into detail about the simple technique I have developed over twenty years of real world practice as a respiratory therapist. It is my hope that I will be able to pass on valuable information which will assist others in becoming more competent, more quickly than if they had to go through countless intubation attempts in order to get a real “feel” for it. I hope this information will help you perform more confidently and competently right from the start, and alleviate much of the stress you are bound to experience as you perfect your own technique.
In addition to the pointers I am offering here, I highly suggest that new intubators find a mentor wherever they will be working who can help them as they begin the process of perfecting their intubation technique. When I was a young therapist, I befriended a very experienced Emergency Room physician and asked him if he wouldn’t mind walking me through the process a few times when appropriate occasions arose. His assistance was extremely helpful and, before long, I began to feel much more comfortable intubating. Eventually, I became experienced enough so that, when an emergency intubation was necessary, he would just let me do it. So, don’t be afraid to approach a more experienced person and express interest in learning the procedure. Doctors, more experienced respiratory therapists, and even anesthesiologists or CRNA’s will usually be happy to help a sincere newcomer. Between that and utilizing the information I am providing you with now, there is no reason you cannot gain the expertise necessary to feel completely confident in performing this life saving procedure.
Intubation Technique
All of the studying is over, all of the necessary preparations have been made, and now you find yourself in the Emergency Room after the “Code Blue” has been called. The emergency medical personnel are wheeling in the patient at a brisk pace. The E.R. nurse has already informed you that the ambulance crew had been called to the scene of an adult male having a heart attack and, on the way to the hospital, he has gone into full-blown cardio-pulmonary arrest. They are currently “bagging” him with a bag-valve device with an attached mask and performing chest compressions, but have not had time to intubate. The time has come. Every member of the team is scurrying about preparing to begin this resuscitation attempt, and here you stand, the person responsible for establishing and protecting this patient’s airway.
In the short time you have been waiting for the patient to arrive, you have already prepared all of the necessary supplies and equipment (as described above). Having covered all of your bases with intense attention to detail during the preparation phase, you feel as confident and ready as you possibly can under the circumstances. Having prepared completely and thoroughly, you are now distraction free. In fact, you might be surprised to be experiencing this level of concentration and focus. But there is no time to fully consider this, because a dying person will be before you shortly and they need your help.
To perform the intubation, you need to be positioned at the head of the bed. Knowing this, you have pulled the stretcher far enough away from the wall so that you can fit comfortably between it and the wall. Once the patient has arrived and been transferred onto the stretcher, the ambulance person who has been bagging the patient hands you the ambu-bag so that you may resume bagging them. Immediately, hook the ambu-bag tubing up to the oxygen flow meter in the wall behind you and ensure it is on and running at 15 LPM or higher. (Make a mental note right now to make absolutely sure you are using the oxygen flow meter and not the compressed air flow meter.) As the emergency medical crew unhooks the patient from their mobile telemetry unit and prepares to remove their stretcher from the resuscitation area, your team members will be moving in to hook the patient up to hospital telemetry, attend to starting IV’s or transferring existing IV’s over to hospital pumps, and attaching a pulse-oximeter probe.
It’s worth re-stating that you don’t want to get overly focused on what the other team members are doing. Now is the time to focus in on what you are here to do. Focus on the patient’s airway, and whether or not you are able to deliver effective rescue breaths with the ambu-bag. In particular, ensure the patient’s head and neck are positioned properly so that there is no positional obstruction to air flow in the airway, and inspect the patient’s oropharynx and mouth for the presence of secretions or vomit that may need to be cleared with suction prior to intubation. You should be able to deliver the rescue breaths without too much resistance felt within the ambu-bag, and with each breath you should see equal and bilateral chest rise movement. If this is the case, continue effective bagging until the patient’s oxygen saturation reaches at least 90% or higher, if possible.
Once the patient’s 02Sat has reached that level, you are ready to attempt intubation. Remember, you only have about 30 seconds to perform the procedure, so move quickly and efficiently. As described above in the preparation discussion, you should already have everything you need within reach and in proper working order. Occasions will arise in which the Code Blue happens so fast and unexpectedly you will not have time to have everything laid out and ready. In this case, once you are ready to intubate, simply ask a team member to continue bagging for you while you quickly gather the required equipment and supplies.
Inserting the Laryngoscope Blade
Standing at the head of the bed bagging the patient, have a team member raise the level of the bed to a comfortable level for you, so that you won’t have to attempt the intubation while stooping down into an uncomfortable position. As the stretcher rises, position the patient’s head and neck into the “sniffing position”. Now is your final opportunity to inspect the patient’s mouth and oropharyngeal space for any obstructions such as false teeth or secretions that will need to be removed prior to intubation. If present, remove false teeth or suction out the airway. When all of this has been done, and the patient has been bagged to appropriately high oxygen saturation, you are ready to intubate.
At this point, I would like to interject a little discussion on laryngoscope blade-type selection. As you know, there are both curved and straight style laryngoscope blades. I am going to assume you have prior knowledge of the technical differences in these blades due to your prior training, so I won’t bore you with a long discussion about that. However, I am going to discuss my preference between the two, and how that preference plays into the technique I am about to explain. I wish I had a dollar for every time I heard someone say, in regards to blade style selection, “It doesn’t matter. It’s really just personal preference” or “Whichever style you first intubate successfully with will be the style you use throughout your career”. Forget all of that, and allow me to explain the practical reasons why I choose to intubate with the long, straight (Miller #4) laryngoscope blade (and, of course, smaller sized straight blades for children or infants).
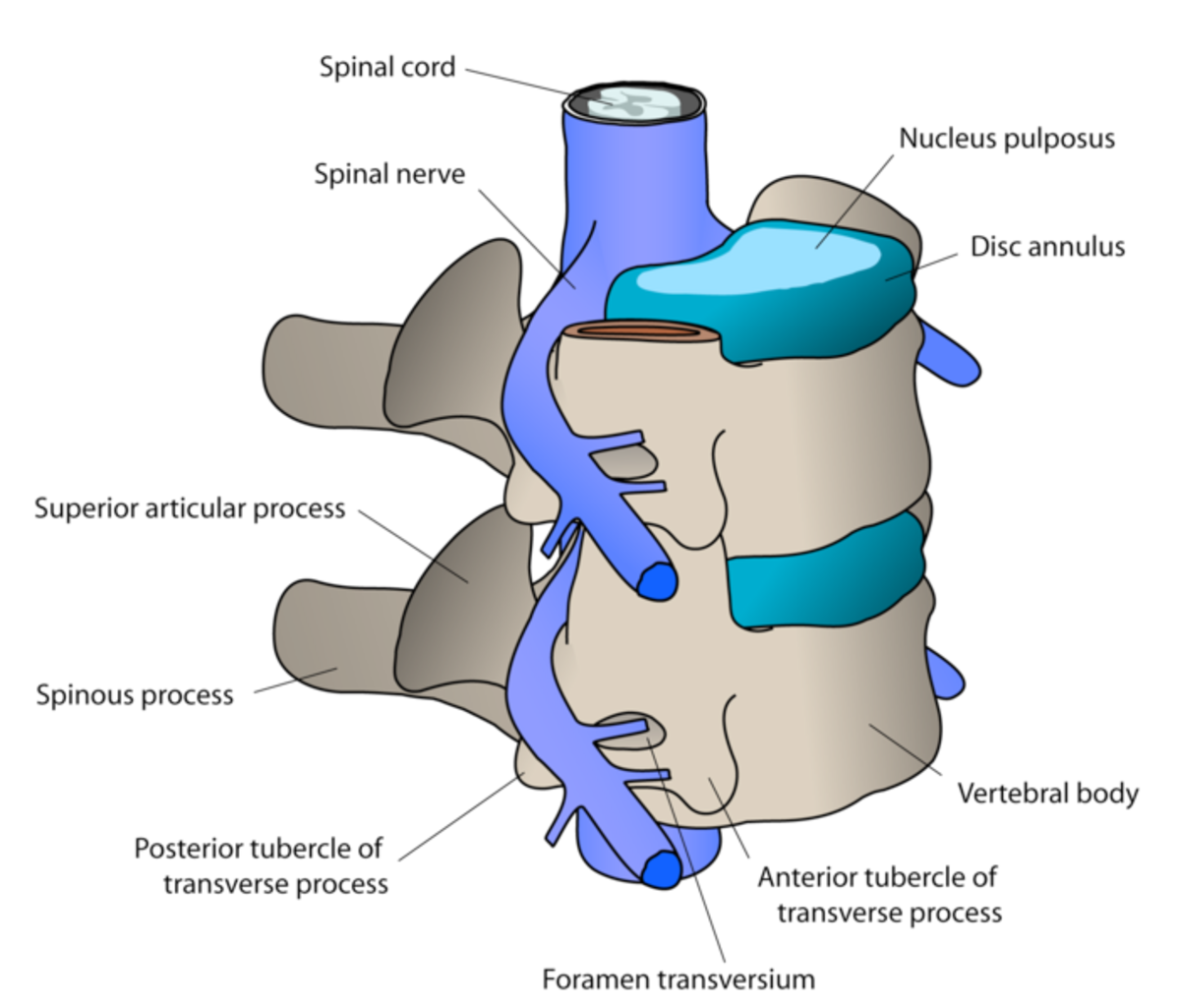
I prefer to use the long, straight blade (Miller #4) for adults because this blade directly lifts the epiglottis (and everything else) to expose the airway, as opposed to the indirect method of opening the glottis that is necessary when using the curved blades. Not only do I take into consideration the direct view into the trachea that a long, straight blade affords but, also, I choose the blade with the widest width and largest “C”-curvature as you are peering down the length of the blade into the airway. In other words, if I have a choice between two straight blades I will always choose the one that is designed to offer the widest and most open view into the airway. Some blade manufacturers offer blades that are designed with a very narrow curvature as you peer down the length of the blade, and I avoid using these if at all possible because of the limited opening (and thus limited view) they provide into the fleshy oropharynx. You are going to find that, in a real human body positioned on its back for intubation, very often, the tongue and flesh inside the mouth and throat present much more of an obstacle to finding the airway than you may have imagined due to the totally relaxed musculature of an unconscious human being. Imagine how, when you fall asleep, your mouth, tongue, and back of the throat will totally relax and cause you to drool or snore. Try totally relaxing the flesh in your mouth and throat right now and notice how the flesh seems to fill up the throat and mouth. Now, consider this in your unconscious patient, throw in a little vomit, blood, or God knows what, and you will begin to get an idea of how difficult it can be to gain visual access to the trachea. I have already discussed the overly pliable, fleshy nature of a real, human airway above. Now we are at the point in this process where all of those factors come into play. Flash back to the head of the bed, standing over your patient ready for your first intubation attempt.
Due to the design of the laryngoscope handle and blades, you must grab the handle in your left hand, regardless if you are right or left-handed. So, with laryngoscope in hand, standing over the patient at the head of the bed as they are lying on their back, insert the long, wide, straight blade into the bottom right point of their mouth as you are viewing it. In other words, as you are viewing their mouth (upside down), insert the blade into the mouth at about the “four O’clock” position. Remembering that you only have 30 seconds to complete the entire procedure, insert the blade deeply and quickly. In fact, insert the long, straight blade slightly further than you know you will need to, so that the tip of the blade actually extends into the esophagus a little past the epiglottis. Now, lift the laryngoscope handle straight up and sweep to the left in a smooth, single motion. This “up and to the left” motion will effectively sweep the fleshy tongue to the left and greatly open up your view deeper into the airway. Remember, at this point you need to have suction close by in order to clear any secretions or foreign matter that may obscure your view of the trachea. Also, remember to lift the laryngoscope handle straight upward, and be sure not to use a prying motion, in order to avoid breaking any teeth or damaging the lips. Keep in mind that, as bad as it would be to break someone’s tooth out, it would be even worse under these circumstances to introduce a broken tooth into the trachea which could effectively obstruct the airway.
Having inserted the blade into the mouth at four O’clock, and introduced it to a depth a little past the epiglottis into the esophagus, lift the handle straight up and to the left moving the tongue out of the way to the left. Avoid any prying motion, and finally make sure the mouth and throat are clear of secretions with suction if necessary. You are, now, able to observe the patient’s oropharynx with the light on the end of the blade. In a perfect world, you will see a perfect view of the open trachea framed with the white triangle of the vocal cords. If you get that lucky, hold your position with the left hand and insert the E.T. tube with your right hand. It does happen that easily sometimes, so be sure to enjoy it if it does because, more often than not, it won’t be that easy.
As I stated above, I insert the blade a little deeper than necessary. That way, after I have lifted the handle straight up, sweeping the blade to the left to open up the view, I will find myself looking into the esophagus. Holding that general position I, then, very carefully begin to withdraw the blade. If the trachea and epiglottis is normal and midline the way all of those pretty textbook pictures show them to be, once I withdraw the blade to the point of the epiglottis, the outward motion of the blade will easily lift it right open and provide me with a straight shot between the vocal cords and into the trachea. And when it does, it’s wonderful! However, as I stated above, probably about thirty percent of the people you attempt to intubate will not have picture-perfect anatomical landmarks. Often, the trachea is deviated to the left or the right. In this case, when you carefully withdraw the blade it will not open up a nice view for an easy intubation. This is where the simple effectiveness of my technique comes into play.
If, having performed your attempt as described above, you find that the patient’s trachea is deviated, you will need to quickly determine where it is, to the left or right. So, without removing the blade from the patient’s oropharynx, reinsert the blade with the same technique as before, however, this time reach up to the patients cricoid cartilage (or Adam’s Apple) with your right hand and grasp it with your fingers (almost as if you were going to choke them) and pull the entire airway to the right and hold it there. Then, as before, carefully withdraw the blade with the left hand. If the trachea is deviated to the left, as you pull back on the blade it will open up the epiglottis and reveal a clear shot into the airway through which you can complete the intubation. If this doesn’t work, simply reinsert the blade again, as before, except this time reach up with your right hand and push the airway over to the left and hold it there as you repeat the same technique of carefully withdrawing the blade. If the trachea is deviated to the right, as you withdraw the blade you will open the epiglottis and reveal a clear shot into the trachea. Understand that this three-in-one technique is to be completed as a single intubation attempt within thirty seconds without ever fully removing the laryngoscope blade from the mouth. You do not remove the laryngoscope and bag the patient each time but, rather, all three “procedures” are to be performed quickly and efficiently within one intubation attempt. Performed correctly, I guarantee you, that you will complete the intubation successfully about 95% of the time on your first attempt. I hate to be the bearer of bad news but, about 5% of those you attempt to intubate will be so anatomically irregular, whether it’s due to deformation, trauma, or swelling, you will have to try more than once to intubate them. I try three times and if I can’t get it, I step aside and let someone else try. Using the technique I describe above, I have had about a 99% success rate with intubations on my first try.
Inserting the E.T. Tube
Although the above technique may sound detailed, getting to the point of having a clear visual shot into the trachea is only half the battle. Once the trachea is visualized, you must now insert the E.T. Tube to the proper depth, get the stylette removed, inflate the cuff, and secure the tube so that it will be supported in place with enough strength to hook the patient up to a life support ventilator and avoid accidental extubation. As you may have expected, there is a trick to that, and I would like to offer you some pointers to help you complete this task easily and efficiently.
Once you have used the above technique with the laryngoscope and successfully opened up your view into the trachea, you will need to carefully hold that position with your left hand while taking the E.T. tube with your right hand and placing it into the airway. As previously stated, the properly sized E.T. tube will have been tested, and lubricated, and have the stylette already placed within it, and the cuffed end of the tube bent to hold about a 45 degree angle on the last two inches of the tube before the intubation attempt. Often, a team member will hand you the pre-prepared E.T. tube in order to help you maintain visual focus on the trachea. This is a critical moment during the intubation, so I want you to be aware of a few things to help you avoid some common mistakes.
First of all, be aware that your view into the trachea at this point will be a small “window”, so you must insert the E.T. tube into the mouth in a way that it will not obstruct your view. To this end, you will need to insert the E.T. tube into the mouth at the same four O’clock position at the bottom, right portion of the mouth opening where you originally placed the laryngoscope blade. Be sure, as you advance the tube toward the trachea, that you slide the tube along the right side of the mouth wall, even stretching the fleshy right side of the mouth wall outward in order to always maintain your unobstructed view of the trachea opening. As you advance the E.T. tube toward the trachea, you will begin to see one of the advantages of having bent the last two inches of the tube with the stylette. Coming in at an angle toward the trachea, stretching the right side of the mouth wall outward to the right in order to maintain your visual on the trachea, you will see, when you have reached the trachea opening at the epiglottis and vocal chords, that the last two inches of the tube bent at a forty five degree angle will be lined up to slide straight into the airway. At this point, go ahead and slide the E.T. tube into the trachea just deep enough so that the proximal end of the cuff goes about ¼ inch past the vocal cords (for any adult or pediatric patient, neonates the depth is much smaller). Note that, no matter the size of the adult or pediatric patient, if you watch the cuff go about ¼ inch past the vocal cords, you will have perfect E.T. tube placement about 95% of the time. Any deeper and you risk inserting the E.T. tube too far, into the right, main stem bronchus. This will result in only the right lung being oxygenated and ventilated, and be less than optimal.
Before I get too far ahead of myself, let’s move back to the spot where you are inserting the E.T. tube into the mouth to attempt the intubation while you are maintaining the opened trachea view with the laryngoscope in your left hand. A very common mistake that new intubators make is to try to slide the E.T. tube directly into and downward along the “C”-shaped curvature of the laryngoscope blade and into the trachea. Don’t ever do this! You will find immediately that you have completely obstructed your view into the trachea with the E.T. tube. You will have, effectively, turned a perfectly open view to the trachea into a blind intubation attempt and greatly lowered your chances for a successful intubation. Also, sliding the cuffed end of the E.T. tube down along the sharp edges of the laryngoscope blade can damage the cuff and cause a leak, or worse yet, a complete failure of the cuff, necessitating re-intubation. Don’t do it.
Another possible difficulty I would like to address at this point is the rare occasion in which you encounter a trachea that is not horizontally deviated to the left or right, but vertically deviated usually upward but sometimes downward (from your viewpoint while intubating). Sometimes the trachea will be, remarkably, even deviated both horizontally and vertically, which results in the ultimate challenge for the intubator. This is another occasion in which having curved the last two inches of the E.T. tube with the stylette will greatly assist you. In my experience, when encountering an airway like this, as I peer down the “C”-curvature of the blade down into the airway, I can actually see the tip of the epiglottis held open by the end of the laryngoscope blade, but there is no view into the trachea because it is abnormally deviated upward. I know that the trachea is open and that it necessarily has to be just under the epiglottis, so I insert the E.T. tube into the mouth as described above but, when the tip of the tube reaches the epiglottis, I use the two inch bend created by the stylette at the end of the tube and turn the curvature upward sliding it directly along the opened epiglottis. If carefully performed, you will be successful at this semi-blind intubation technique about 90% of the time. Paying close attention, you may even hear air moving inside the E.T. tube to help you verify the tube is, indeed, inside the trachea. However, when this type of situation arises, you must verify you have actually, in fact, intubated the trachea and not the esophagus. This is where an ETC02 detector becomes invaluable. Once the cuff is inflated and the stylette is removed from the E.T. tube, (being careful to maintain the position of the tube) place the ETC02 detector onto the proximal end of the E.T. tube and bag the patient through it. If you have successfully intubated the patient, you will notice the inside material of the ETC02 detector will change color as the exhaled carbon dioxide moves across it. If you have erroneously intubated the esophagus, there will be no presence of carbon dioxide and, therefore, no color change within the ETC02 detector. This is a very effective method to verify intubation, but even after this you still need to verify with other traditional methods such as breath sounds and chest X-ray.
Securing the E.T. Tube
Once the E.T. tube has been successfully inserted into the trachea at a depth so that the cuff is about ¼ inch past the vocal cords, the next big priority is to hold the proper positioning of the tube while you quickly remove the laryngoscope from the oropharnx, inflate the cuff to the appropriate pressure, remove the stylette from the tube, and place the ETC02 detector onto the end of the tube to verify placement. The best way to make sure you do not lose E.T. tube placement is to firmly hold the tube between your thumb and index finger right where the tube extends from the corner of the mouth, while resting the palm of the same hand against the patient’s cheek. The hand on the cheek tends to stabilize the E.T. tube, while keeping the fingers pinched onto the tube at the corner of the mouth ensures that you maintain the correct depth, neither proceeding the tube deeper nor receding it to a more shallow position. At this moment, right after the intubation itself, it is a good idea to go ahead and bag the patient, delivering several oxygen-rich rescue breaths to the patient, while remaining extremely careful to maintain the position of the tube with the other hand as described above. While bagging, be especially careful not to displace the E.T. tube. Many less experienced practitioners make the mistake of grabbing the ambu-bag with both hands and fail to retain correct tube placement, or worse, accidentally extubate the patient. Don’t be that person! Hold the E.T. tube with one hand and bag with the other. Once an advantageous increase in oxygen saturation has been attained, use one of the E.T. tube holders to more substantially secure the E.T. tube. As far as E.T. tube holders go, I prefer the kind that has an adjustable, plastic screw which holds the tube into place. I have found them to be greatly reliable, yet easy to adjust tube placement later on should it become necessary. That being said, however, any commercially available type of E.T. tube holder will usually suffice. Some of us old-timers remember when we just used tape to secure the E.T. tube, but I, for one, am happy to see those days gone by. But, if you find yourself suddenly needing to secure an E.T. tube and don’t have a commercial tube holder available, know that you can successfully secure it with tape, just be very careful to do it cautiously (so as not to lose proper tube placement) and securely.
Post-Intubation
After all of the above has been successfully completed you can, now, bag the patient through the E.T. tube. Again, be sure to go through all of the proper E.T. tube placement verification such as bilateral breath sounds, ETC02 detector color change, condensation in the tube, increasing 02Sats, and chest X-ray. With placement verified and tube strongly secured, you simply continue to bag the patient, providing rescue breaths until, either, the Code is called or it becomes necessary to transfer the patient from the ambu-bag to the life support ventilator.
Conclusion
Hopefully, all of the information provided here will give you enough specific information to help avoid many of the pitfalls experienced by less experienced intubators. Looking back on all of the details mentioned herein, I am struck by just how many details need to be attended to for a procedure that last no more than 15-30 seconds. Take heart! We all were beginners once and, armed with this information, I feel sure that you will be much more successful at this procedure, much more quickly! Now get out there and save some lives! Good luck!
If You Found This Helpful…
Please, take a few moments to click on the links of some of the advertisers on these pages. This will be very helpful for the author! Thank you!